(RxWiki News) Results from the first clinical trial of a drug designed to treat advanced cases of melanoma were successful, and the second part of testing has been approved.
A three-year trial concluded this May, testing how effective the melanoma drug, dabrafenib is in treating advanced solid tumors, including those with metastasis.
Dabrafenib works specifically in tumors with a mutation in a gene called BRAF, which is common in melanomas.
"Ask your oncologist about clinical trials."
Researchers from MD Anderson stated that this is the most successful trial to date with melanoma cancers that have begun to grow in the brain.
There is no current standard treatment for brain metastasis in melanoma. Understandably, metastasis is a dangerous complication for any cancer, but undetected and untreated melanoma metastasis is particularly difficult to treat.
The purpose of this study was to judge whether the drug had any effect, and also to find out at what point the drug becomes dangerous. This research was needed to determine the best range of doses to use for the next part of testing, referred to as phase two.
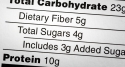
The trial used data from 184 patients with incurable solid melanomas, 156 of which had metastatic tumors. The 156 patients with metastatic melanoma are given escalating doses of dabrafenib. The investigators concluded phase one by deciding to use two doses of 150 mg per day as the baseline for the phase two testing.
The third phase of testing usually compares the experimental treatment to the current gold standard, but since metastatic melanoma has no successful treatments, another measurement will be used.
The fourth and final phase of drug testing will occur if the drug is approved by the FDA. This is the period where the drug is made available for public use, and doctors send periodic updates back to pharmaceutical companies.
Information is collected from the much larger number of patients who are being exposed to the drug, and the company looks for rare side effects as well as unusual and unpredicted drug interactions.
"Brain metastases in most [nine of ten] patients given dabrafenib reduced in size, with four patients' metastases completely resolving", says study author, Gerald Falchook MD from the University of Texas MD Anderson Cancer Center.
Dr. Falchook went on to describe the study results,"Patients with melanoma and brain metastases typically survive for less than 5 months; yet in this study, all ten patients were alive at this stage and two patients had durable antitumour activity with survival beyond 12 months. One patient remains on treatment at 19 months".
During the initial research and development of the drug, there has been some activity against other cancers with mutations in the BRAF gene, including cancers in the lung, colon, thyroid and ovaries.
While the drug was designed to be effective only in patients with a mutation for the BRAF protein, in this study, researchers found that it was also effective in 4 of 18 patients who had a different mutation other than in the BRAF gene.
So far, some serious side effects revealed in this phase of drug testing include a minor form of skin cancer called cutaneous squamous-cell carcinoma, severe fever and fatigue, occurring in slightly more than one out of ten patients.
The authors concluded the study by outlining the effectiveness of the drug and the need to continue clinical trials in larger groups to understand the full abilities of the drug.
Published next to the study in The Lancet was a commentary by Geoffrey Gibney, MD stating, "[These findings] are impressive for two reasons: no previous systemic treatment has shown this degree of clinical activity against melanoma brain metastases, and dabrafenib was not predicted to cross the blood-brain barrier in substantial quantities…"
"Overall, the prospects for use of BRAF-targeted treatment in new patient populations are encouraging."
The study was published in the May edition of The Lancet. Funding for this study was provided by pharmaceutical multinational GlaxoSmithKline.