(RxWiki News) Computer scans can help doctors pinpoint targets for surgery, treatment or see if cancer is on the move. One technology has proved to be very accurate for people living with melanoma.
A recent study tested computer-aided scans to see how well they located tricky melanomas spreading to lymph nodes.
The scans helped doctors find sentinel lymph nodes for easier removal and longer lasting cancer remission.
"Get checked for skin cancer regularly."
Ingo Stoffels, MD, from the Department of Dermatology at the University School of Medicine Essen-Duisburg in Essen, Germany, led the study.
Researchers were looking for a way to use a non-invasive, computer-aided scan called single-photon emission computed tomography/computed tomography (SPECT/CT) to find melanoma in sentinel lymph nodes.
Usually this is done with what’s called a sentinel lymph node excision (SLNE). Doctors remove lymph nodes closest to the tumor to see if they contain cancer.
Previous research has shown that melanoma patients with no cancer in the sentinel lymph node had less than a 5 percent chance of having cancer in any lymph nodes.
Researchers found more sentinel lymph nodes (SLN), used less invasive surgery to remove the SLN and lengthened remission time in melanoma patients with SPECT/CT scans.
This is great news—because it means this targeted scan can determine the presence of cancer rather than an invasive surgery alone to find, remove or biopsy SNL.
Using a SPECT/CT scan can also help lower the rates of false negatives from SLNE procedures.
For the study, 464 melanomas were comparatively tested from 2003 to 2011 to see if the SPECT/CT scans were as effective as SLNE procedures in detecting melanoma in the lymph nodes.
The SPECT/CT scans allowed doctors to find 21 percent more sentinel lymph nodes in the head and neck area more easily than SLNEs alone.
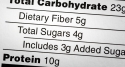
The study found that SPECT/CT scans were more effective than SLNEs in a number of other areas, including:
- Locating 21 percent more SNLs in the head and neck area.
- Detecting more SNLs per patients than SNLE alone, 2.4 vs. 1.87.
- Detecting more cancer positive SNLs than SNLE alone, 0.34 vs. 0.21.
- Improving relapse rates – 7 percent vs. 24 percent for SNLE group.
These lower relapse rates extended the lives of patients. An average of 94 percent of those in the SPECT/CT group were disease free after 4 years, compared with 79 percent of patients who had SNLE.
Overall, 833 sentinel lymph nodes were removed from 403 patients with 14 percent in the SPECT/CT and 11 percent in the SNLE tumors starting to spread.
The SPECT/CT scans allowed researchers to use smaller incision areas to remove sentinel lymph nodes that had been clearly imaged.
Authors concluded that using the SPECT/CT was helpful in accurate detection of melanoma in sentinel lymph nodes with less invasive surgery techniques and better rates of disease-free post-operation years.
SPECT/CT scans are widely available in hospitals and generally cost between $500-$1000.
This study was published in September in the Journal of the American Medical Association.
No funding was provided to support this study.
Dr. Schadendorf has received lecture and consulting fees from various pharmaceutical companies, but no conflicts of interest were reported by any of the authors.