(RxWiki News) For the last fifty years, very few treatments have been available for advanced cases of melanoma, but several new drugs in the final stages of development are in competition for the title of best treatment.
The results from two studies presented to the American Society of Clinical Oncology found that the effectiveness of dabrafenib exceeded expectations for advanced melanoma therapy, and was shown to be effective in cases of metastasis to the brain, with an acceptable level of side effects.
"Ask your oncologist about the latest treatments available for your cancer."
A study by Axel Hauschild, MD, from the Universitaetsklinikum Schleswig-Holstein in Kiel, Germany found that using dabrafenib stopped the growth of melanoma in patients for 70 percent longer than the standard treatment using chemotherapy.
Evaluations of the side effects of dabrafenib compared to the other melanoma drugs targeting BRAF mutations have shown dabrafenib to have the upper hand so far.
"For BRAF-mutated patients, standard of care is no longer DTIC. Each and every patient needs to be offered a BRAF inhibitor," Dr. Hauschild stated during his presentation. "It's the beginning of a completely new era in treatment of metastatic melanoma."
The BREAK-3 trial included 250 patients with stage III, V600E-mutated metastatic melanoma randomized to 150 mg of dabrafenib twice daily or 1,000 mg of IV dacarbazine chemotherapy every 3 weeks, with the option to cross over at signs of disease progression.
As reported in the study, the average time for evidence of advancing cancer growth was 5.1 months when patients were treated with dabrafenib, in comparison to an average of 2.7 months with the current standard chemotherapy, dacarbazine.
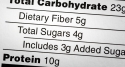
While not all data was given, the respective response rates for dabrafenib vs. chemotherapy were as follows.
- Complete response: 3 vs. 0 percent
- Partial response: 50 vs. 19 percent
- Stabilization: 40 vs. 30 percent
Dr. Hauschild stated that presenting the overall survival results were premature since the majority of the patients enrolled in the study were still doing well.
Final data from the study on brain metastasis was also withheld, but study authors stated that the clinical effectiveness of dabrafenib in these cases was significant, with high levels of activity against the cancer.
The most common side effects noted in the clinical trials of dabrafenib have been the development of hardened, thickened skin, a condition known as hyperkeratosis which occurred in 72 percent of patients.
Joint pain, fatigue, and headache were not as common, reported by less than a quarter of patients.
The drug's manufacturer, GlaxoSmithKline, announced plans to apply for FDA approval of dabrafenib for treatment of metastatic melanoma as well as another drug under development, trametinib, which targets another pathway involved in several skin cancers.
Dr. Hauschild mentioned another study recently completed that showed promise using both of these drugs as a combination therapy for melanoma, and wished to further study the effects of combination therapy.
"The next step is the combination of BRAF and MEK inhibition with dabrafenib and trametinib, not only for stage IV but also in the adjuvant setting."
The moderator at the ASCO press conference, Sylvia Adams, MD, of New York University Langone Medical Center, spoke after the presentation. "The results from the BREAK-3 trial confirms that BRAF targeting is effective, but may give dabrafenib the edge with regard to safety."
Dabrafenib targets a mutation in the BRAF gene known as V600E. Several studies have shown that over half of advanced melanomas have a mutation in the BRAF gene, and the V600E is the most common variation.
Researchers estimate that roughly a quarter of metastatic melanomas patients would be eligible for this targeted treatment.
Study data presented at conferences is considered preliminary until published in a peer-reviewed journal.
Funding for the study was provided by the manufacturer, GlaxoSmithKline, and researchers disclosed financial ties, employment, and stock ownership with that company as well as Bristol Meyers Squibb, Roche, Bayer, and Novartis.