(RxWiki News) It’s not just how much you eat, it also may be what you eat that matters when it comes to living beyond cancer. A new study shows this very likely is true for colon cancer patients.
Former colon cancer patients who eat a diet high in sugars and carbs are more likely to see their disease return than survivors who have more balanced diets.
Folks who are overweight or obese and eat this way are at highest risk.
"Cut down on sugar."
A recent multi-institutional study examined the diets of more than 1,000 patients with advanced stage III colon cancer.
While the findings point to a connection between diet and relapse, the authors say their findings aren’t conclusive.
Lead author, Jeffrey Meyerhardt, MD, MPH, associate professor of medicine at Harvard Medical School, said in a news release “Our study certainly supports the idea that diet can impact the progression of colon cancer, and that patients and their doctors should consider this when making post-treatment plans. But further research is needed to confirm our findings.”
Other studies have found that cancer winners whose diets elevate insulin levels are more likely to have the cancer return. Insulin levels are increased by eating starchy, sugary foods.
A total of 1,011 stage III colon cancer patients took part in this study. They had been treated with surgery and participated in a trial looking at the after-effects of chemotherapy.
Study members filled out surveys about their diets for six months following treatment.
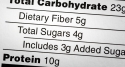
Investigators kept track of the total carbohydrate intake of everyone. They also looked at the glycemic index, which measures how food affects blood sugar levels, and glycemic load, which measures the amount of carbohydrate in food.
Patients who consumed the highest levels of carbs and glycemic load had an 80 percent increased risk of a cancer recurrence or death compared to patients who consumed the lowest levels of carbs.
Those who had a body mass index of above 25 had even higher risks of recurrence or death.
"In light of our and other’s research, we theorize that factors including a high glycemic load may stimulate the body’s production of insulin,” Dr. Meyerhardt said.
“That, in turn, may increase the proliferation of cells and prevent the natural cell-death process in cancer cells that have metastasized from their original site.”
He cautioned that this study doesn’t prove a connection, but suggests the findings “...offer useful guidance for patients and physicians in ways of improving patient survival after treatment.”
In addition to Dana-Farber, researchers from Duke University Medical Center, Memorial Sloan-Kettering Cancer Center, Toledo Community Hospital Oncology Program, Toledo, OH, Hôpital du Sacré-Coeur de Montréal, Canada, Loyola University Stritch School of Medicine, Northwestern University and the University of California at San Francisco were involved in this work.
The research was funded by the National Cancer Institute grants, a GI SPORE grant and Pfizer Oncology.
The findings are being published online November 7 by the Journal of the National Cancer Institute and will appear later in the journal’s print edition.
No conflicts of interest were reported.