(RxWiki News) Concerns about child and teen obesity are not new, but they have been growing. In particular, the number of youth who are severely obese is increasing.
A recent statement published by the American Heart Association focused on the growing problem of severe obesity among youth.
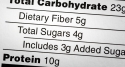
The most common definition for "severe obesity" among youth is having a body mass index at or above the 99th percentile for a person's age and height. Body mass index, or BMI, is a ratio of a person's height to weight and is used to determine whether they have a healthy weight.
The statement reviews what treatments exist and the short-term and long-term risk factors for other health problems associated with severe obesity.
"Discuss your child's weight with a pediatrician."
The statement, written by an American Heart Association committee led by Aaron S. Kelly, PhD, of the University of Minnesota Medical School, discussed the growing problem of severe obesity among youth.
The authors report that somewhere between 4 and 6 percent of all youth in the US suffer from severe obesity and that these numbers are increasing.
An even greater problem, however, is that few treatments exist with long-term effectiveness and wide availability to teens.
One treatment that has shown some limited success involves lifestyle and behavior modifications, but these are very involved and are difficult to maintain over longer periods of time.
Participants in these programs have frequently lowered their BMI, "...but participants have generally remained severely obese and often regained weight after the conclusion of the treatment programs," the authors wrote.
Currently, only one medication, called Orlistat, has been approved by the FDA for treating obesity in adolescents, so not many medication options are available.
Even with Orlistat, the weight loss teens experience is not huge, and side effects, such as needing to use the bathroom suddenly and having abdominal pain, can be unpleasant.
Another option for treatment is bariatric surgery, which involves surgically restricting a person's stomach or similar digestive system modifications.
While this treatment has shown to be effective in reducing teens' body mass index and risk factors related to heart and metabolic health, the treatment is not appropriate for everyone.
Many teens with severe obesity may not qualify for the surgery based on certain characteristics. In addition, the surgery is expensive and therefore generally only available to teens with sufficient health insurance.
Also, not much long-term research data exists to show how these young people do much later on once they have had bariatric surgery.
Due to this growing problem with severe obesity among American youth, the authors proposed a standardized definition for severe obesity in children and teens and then presented information based on the current research about risk factors and long-term outcomes for the severely obese.
Regarding the definition of severe obesity, the authors proposed that other possibilities be considered for a standardized definition besides the 99th percentile definition.
Although obesity can also be measured in terms of skinfold thickness or waist circumference measures, the authors discouraged these measures because they are not always available and/or are subject to error.
Instead, the authors recommended defining severe obesity in children/teens aged 2 and older as having a BMI of 35 or having a BMI of 120 percent or greater of the 95th percentile, whichever is lower.
Currently, having a BMI of 35 is considered severe obesity in adults. A BMI of 30 to 34.5 is considered obese, and a BMI of 25 to 29.9 is considered overweight in adults.
The authors also reviewed the health risks associated with severe obesity in teens.
These risks include increased blood pressure, insulin resistance, increased inflammation and changes to the circulatory system that can increase the risk for heart disease.
Inflammation refers to an irritation of tissues in the body that is linked to various diseases or health conditions. Insulin resistance is an early warning sign and risk factor for developing type 2 diabetes.
Other health conditions that can develop as a result of severe obesity include obstructive sleep apnea (stopping breathing and/or getting insufficient oxygen while asleep), fatty liver disease and musculoskeletal problems such as knee pain or greater risk of fractures.
In addition, children who are severely obese are at greater risk for psychological or social problems, as well as for eating disorders, the authors noted.
The researchers therefore emphasized the importance of seeking more treatments that are effective for children with severe obesity.
This need would involve greater research into behavioral programs, medications and other options that might be effective for the longer term.
This statement was published September 9 in the journal Circulation. No external funding was reported for the paper.
The lead author has received research support from Amylin Pharmaceuticals and Thrasher Research Fund. One other author has received research funds from Ethicon Endosurgery, and a third author has received research funds from Takeda Pharmaceutical Company, Inc.