Feeling a little tired at the end of your day is normal. But if you've been feeling exhausted for weeks or months on end, even after what seemed like a good night's rest, you could have a blood disorder known as anemia.
However, exhaustion is not the only sign of anemia. Before you go ahead and accept you have anemia, you should learn about the condition. Knowing the signs and symptoms can help you and your doctor figure out what's causing your anemia and how best to treat it.
What is anemia?
Anemia is one of the most common blood disorders in the United States, affecting more than three million Americans. While there are many different types of anemia, they all share some common characteristics.
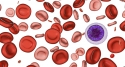
Anemia occurs when you do not have enough healthy red blood cells to carry oxygen to the body's tissues. If you have anemia, this lack of oxygen can give rise to a variety of symptoms, including the following:
- Fatigue
- Weakness
- Shortness of breath
- Pale skin
- Dizziness
- Fast or irregular heartbeat
- Chest pain
- Pale skin
- Pounding or "whooshing" in your ears
- Cognitive problems
"Fatigue and paleness to the skin and eyes can be signs of anemia," explains Chris Galloway, MD, a dailyRx expert who specializes in emergency medicine. "Mild iron deficiency anemia can usually be easily treated, but some other acute forms of anemia can be much more serious. If you are feeling new onset of these symptoms, schedule an appointment with your doctor to be checked. A simple blood count (CBC) is all that is needed."
In some cases, the symptoms of anemia are so faint that the condition can be hard to notice. But as anemia worsens, symptoms can increase in number and intensity.
What causes anemia?
At the root of anemia is a lack of healthy red blood cells. Red blood cells contain hemoglobin, an iron-rich protein that helps carry oxygen from the lungs to tissues throughout the entire body.
Problems with red blood cells typically arise due to the following:
- Your body damages or destroys red blood cells.
- Your body does not produce enough red blood cells.
- Through bleeding, you lose red blood cells more quickly than your body can replace them.
These issues with red blood cells lead to virtually all types of anemia. Common types of anemia include the following:
- Iron deficiency anemia. Most anemia patients have this form of the condition. Iron deficiency anemia occurs when your body does not have enough iron. Low iron is usually caused by blood loss but can also result from poor absorption of iron.
- Vitamin deficiency anemias. Your body not only needs iron to make healthy red blood cells but also folate and vitamin B-12. If you don't have enough of these vitamins, your body may produce fewer red blood cells. In many cases, folate or vitamin B-12 deficiency is due to poor diet. However, some people may consume enough B-12, but their bodies cannot properly absorb it.
- Aplastic anemia. This is a rare but potentially life-threatening form of anemia. Aplastic anemia occurs when the body loses the ability to make enough red blood cells. Common causes of aplastic anemia include infections, exposure to toxic chemicals, drugs and autoimmune diseases.
- Hemolytic anemias. These types of anemia occur when red blood cells are destroyed faster than they can be replaced. Hemolytic anemias can be caused by leaky heart valves, aneurysms (abnormal ballooning of the blood vessel), infections, autoimmune diseases or birth defects. These anemias can be inherited or may develop later in life.
- Sickle cell anemia. This is an inherited form of anemia that, in some cases, can be serious. Sickle cell anemia is caused by an abnormal type of hemoglobin that causes red blood cells to take on a "sickle" shape. These misshapen red blood cells can die early, leading to a lack of red blood cells. They can also get caught in the blood vessels and clog blood circulation.
- Anemias caused by other diseases. Some diseases can disrupt your body's ability to produce red blood cells. Such diseases include cancer, HIV/AIDS, rheumatoid arthritis, Crohn's disease and other chronic inflammatory diseases. Kidney disease can also lead to anemia because the kidneys are not making enough erythropoietin, a hormone that signals red blood cell production. Cancers of the blood or bone marrow (e.g., leukemia, multiple myeloma and lymphoma), and the chemotherapy to treat these cancers, can also interfere with the body's ability to make new red blood cells.
Am I at risk for anemia?
You may be at risk of anemia if you have any of the following risk factors:
- A diet lacking in iron, vitamin B-12 or folate
- Intestinal disorders, such as Crohn's disease or celiac disease, which affect the absorption of nutrients
- Surgery or removal of parts of the small intestine that are involved in nutrient absorption
- Pregnancy, in which a woman's iron supply is needed not only for her body but also that of her growing baby
- Heavy periods, which cause loss of red blood cells
- Chronic conditions such as cancer, kidney failure and liver failure among many others
- A family history of anemias that can be inherited, such as sickle cell anemia
- A history of certain infections, blood diseases, autoimmune disorders, alcoholism, exposure to toxic chemicals or use of certain medications
How do I know if I have anemia?
First, it's important to pay attention to your body. If you can't explain why you've been feeling so exhausted or fatigued, you may have anemia.
If you start to notice symptoms of anemia, it may be time to make an appointment with your doctor, who can do a physical exam and run tests to give your a proper diagnosis.
One common test used to diagnose anemia is a complete blood count (CBC). Using this test, your doctor will measure levels of red blood cells (hematocrit) and hemoglobin in your blood. In general, normal hematocrit is considered between 38.8 and 50 percent for adult men and 34.9 and 44.5 percent for adult women. Anemia is typically diagnosed if a CBC shows a hemoglobin value of less than 13.5 grams per deciliter in a man or less than 12 grams per deciliter in a woman.
Another test used in anemia diagnoses determines the size and shape of your red blood cells. Such a test may allow your doctor to identify the specific type of anemia you have. If you have a vitamin deficiency anemia, for example, your doctor may see lower levels of red blood cells that are enlarged.
How is anemia treated?
The treatment you receive will depend on the type of anemia you have.
Iron deficiency anemia is usually treated with dietary changes and iron supplements. But if loss of blood is the cause of your iron deficiency, doctors must find and stop the source of bleeding, which sometimes can require surgery.
Vitamin deficiency anemias are treated with supplements and diets high in the vitamins you lack.
Treating aplastic anemia may require blood transfusions or even a bone marrow transplant.
If you have a hemolytic anemia, you may need to avoid certain medications, get treatment for related infections and take medications that suppress your immune system. In more severe cases of hemolytic anemias, treatment may require a blood transfusion or plasmapheresis (a process to filter blood plasma).
In cases in which the anemia is caused by a chronic disease, treatment typically involves treating the underlying disease.
How can I prevent anemia?
Unfortunately, certain types of anemia cannot be avoided. However, other types of anemia, particularly iron and vitamin deficiency anemias, can be prevented through a diet that includes healthy foods rich in iron, folic acid and vitamin B-12.
The following foods are high in iron:
- beef
- dark green leafy vegetables
- dried fruits
- nuts
The following foods are high in folic acid:
- citrus juices
- dark green leafy vegetables
- legumes
- fortified cereals
Meat and dairy are good sources of vitamin B-12.